Prof. Rūta Navakauskienė: Future of Cancer – Personalised Treatment

“Many cancers are curable with existing protocol therapy, however, not all cancers respond to it. Based on the data of my research, I think that both treatment and diagnostics will become more and more individualised,” says Prof. Rūta Navakauskienė, researcher of Vilnius University Life Sciences Center. Her research group’s study on stem cells and their therapeutic application is part of this progress.
In October 2023, the Lithuanian Academy of Sciences nominated the cycle of works “Investigation of the role of cancer and stem cells in the pathogenesis of diseases and their application for therapy – synergy of experimental biology and computer informatics (2008–2022)” Prof. Rūta Navakauskienė (together with Prof. Dalius Navakauskas, Dr. Veronika Viktorija Borutinskaitė and Prof. Dalius Matuzevičius) as candidate for the Lithuanian Science Prize. We spoke with the professor about her ongoing research and the future of cancer treatment.
You’re conducting a lot of research trying to understand how leukaemia develops and how best to treat it. What do we still not know about leukaemia? What are you trying or would like to learn?
I think we should start with what leukaemia is. It is a cancer of the white blood cells. As with all cancers, it is not known exactly how it occurs. These can be harmful environmental factors, perhaps stress or radiotherapy and chemotherapy, while treating other diseases.
All mature cells in the body are differentiated: that is, they perform a specific function for the organ they form. All the blood cells we know develop from stem cells in the bone marrow. During their differentiation, stem blood cells become mature blood cells that perform their intended function.
During the development of blood cancer, undesirable changes occur at a certain stage of differentiation of blood stem cells, and their differentiation into finally mature cells stops. This can happen due to genetic mutations, altered signalling pathways, or epigenetic changes.
It is also possible that this happens due to a disturbed immune response. In the adult body, if a normal cell or its development is altered, a well-functioning immune system is able to recognise and defeat such cells – so we do not get cancer or other diseases. However, if the immunity is weakened and other factors are involved, the normal development of the cell can be disrupted, and the blood cell begins to multiply uncontrollably, without performing its intended function.
In our research, we focus on unwanted epigenetic changes, which are also very important for normal cell development and functioning. More specifically, we work with acute myeloid leukaemia.
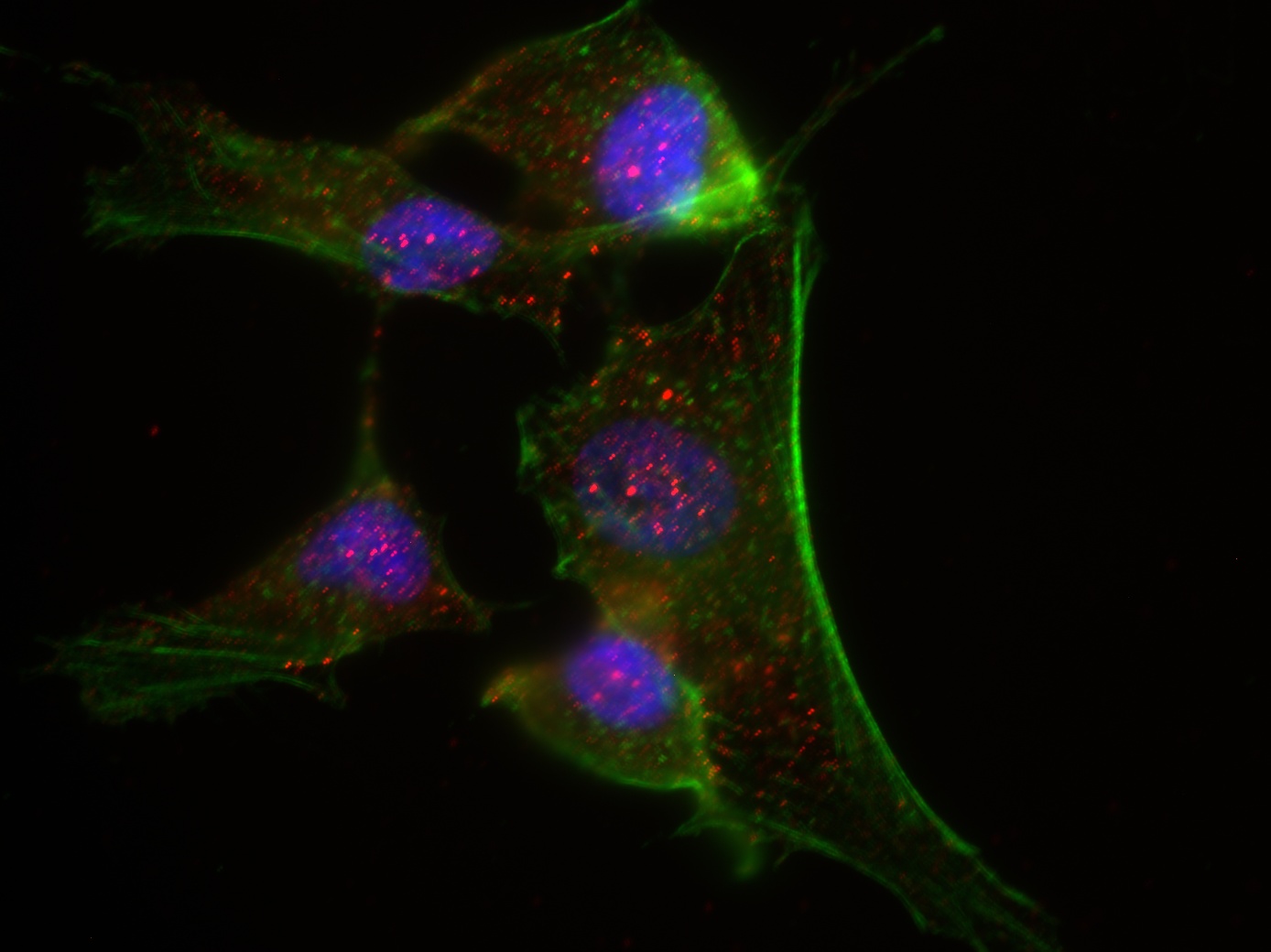
Imaging of protein markers and determination of their localisation in the cell. Photo credit: personal archives
What are the fundamental molecular differences between a healthy stem cell and a cancer cell?
In fact, they have many features in common. The common and distinctive feature is the ability to self-renew, divide and reproduce. But the key difference is that a healthy stem cell can control its own division, while a cancer cell reproduces uncontrollably, resulting in a tumour.
Healthy stem cells differentiate when the body needs mature cells with a specific function. Then, they differentiate into a specific cell of a certain tissue. And the cancer cell does not differentiate, it simply multiplies unstoppably.
As I’ve mentioned, we study epigenetic processes related to stem cell differentiation and the changes that occur in cancer cells. Epigenetic diversity is also important for the body.
What does it mean?
The epigenetic profile of stem cells and their changes during differentiation determine the diversity of those cells. If we were to start from the very beginning, all our cells have the same genomic DNA, but when they differentiate into tissue-specific cells, the genes begin to act completely differently to perform an organ-specific function. This process is regulated by epigenetics.
If epigenetic mechanisms determine the diversity of stem cells, the epigenetic changes in cancer cells determine their turning into cancerous ones. In research, we use various epigenetic modifiers and a combination of them to treat cancer cells, in this case leukemic cells.
The immediate question is, how do you study the characteristics of cells and their potential for treatment?
We conduct molecular studies of healthy and cancerous cells and carry out a comparative analysis of the results obtained: we want to see what is happening in those normal cells and what exactly is the difference between molecular mechanisms in healthy and cancerous cells. We conduct molecular research at the genetic and epigenetic as well as at protein and its modification, that is, proteomic, levels.
In our research, we use commercial cell lines that we purchase from certified cell banks. Scientists all over the world working in this area of research use the same cells. These are in vitro studies.
But we don’t stop here, because during 30 years of research we’ve learned that commercial lines are not the same as those in the body. In collaboration with oncologists-hematologists, we have the opportunity to study cancer cells isolated from the patient (ex vivo). It means that after receiving biological material from a patient with leukaemia, we isolate the cancerous blood cells and analyse them at the molecular level.
We use various epigenetic modifiers and their combinations. We regulate gene expression through epigenetic reprogramming. For this, we use various chemical agents and a differentiation inducer because, as I’ve mentioned, the type of leukaemia we are studying is associated with arrested cell development at a certain stage of differentiation. Therefore, we need to stimulate the cell to induce differentiation into a normal, mature cell. Of course, while evaluating the effectiveness of selected epigenetic combinations in cancer treatment, we also conduct preclinical studies (in vivo) – we use experimental laboratory animals.
Prof. Rūta Navakauskienė. Photo credit: Rūta Andrė
And what animals do you usually use?
The experimental laboratory animals we use are mice. We publish all the results of research in vitro, ex vivo, in vivo (in mice) in highly-ranked international journals. We hope that clinical, biotech commercial and pharmaceutical companies will notice them and move them to clinical trials.
Can you tell us how stem cells can be used in cancer treatment?
The treatment of some forms of blood cancer is confirmed and is carried out by stem cell transplantation. This has been done in Lithuania since 1999. As far as I know, stem cell therapy is used in cases of childhood leukaemias when graft-versus-host-disease develops. T-cell therapy is used more for lymphoblastic leukaemia. Many clinical trials using stem cells are being conducted in other countries, mainly in the United States of America.
Our research group is also looking for alternative sources for stem cells. For this, we use perinatal derivatives and tissues of the reproductive system. These are the placenta, umbilical cord, umbilical cord blood, amniotic fluid, and endometrial tissue. We have also developed methods to isolate those cells.
And these cells are unique in that they are not immunogenic – they can be used for allogeneic transplantation. They have 100% compatibility with another host. According to their characteristics and properties, they are somewhat intermediate between embryonic stem cells and adult human cells.
We have been working with stem cells for over ten years. From the results obtained by our research group and in cooperation with international partners, we can safely say that they can be applied not only to the treatment of cancer but also to many other diseases: pathologies of the reproductive system, congenital pathologies, diagnosis of fetal pathologies, etc.
You’ve mentioned that you get perinatal derivatives. How does this process work? Does the person themselves, such as a pregnant woman, have to agree to share tissues with you?
Yes, that’s right. Since we work with biological material, we have all the necessary permits approved by the Lithuanian Bioethics Committee to conduct biomedical research with biological material. A person who agrees to participate in a biomedical study always signs a consent form. It is only in such a case that biomedical research is possible.
When we talk about amniotic fluid, it is isolated only in cases where there is a suspected pathology of fetal development. It is not taken during normal pregnancy. Our research is carried out in close cooperation with physicians. And I am very pleased to note that in biomedical research, we cooperate closely and mutually in evaluating research results. We believe that this work will also be useful in further clinical studies.
Perhaps, the cooperation of such an interdisciplinary group of researchers, medics, etc., also helps to formulate the problem more clearly. For example, physicians probably see from practice what is needed and then turn to researchers to help solve it.
Yes, that’s right. Speaking about cancer, there are types of cancers that respond to treatment, and patients recover. However, there are such forms that are treatment-resistant. In the case of acute myeloid leukemia that we study, some patients recover, but there are cases where cancer becomes resistant to treatment – we study relapsed/refractory acute myeloid leukemia (R/R AML). In such a case, a personalised treatment appears to be of importance.
In collaboration with oncochematologists, we conducted one study in which we observed that the metabolic activity of patients with poor prognosis differs. For example, in ex vivo studies, we treated patient’s blood cancer cells with changed oxidative phosphorylation state with a drug already known and used to treat both type 2 diabetes and polycystic ovary syndrome. This treatment reduced oxidative phosphorylation. In our study, we demonstrated that the treatment with the mentioned drug has a positive effect on blood cancer cells with changed mitochondrial activity. The results are published in the international journals. These studies demonstrate the importance of personalised treatment based on molecular findings in cancer cells.
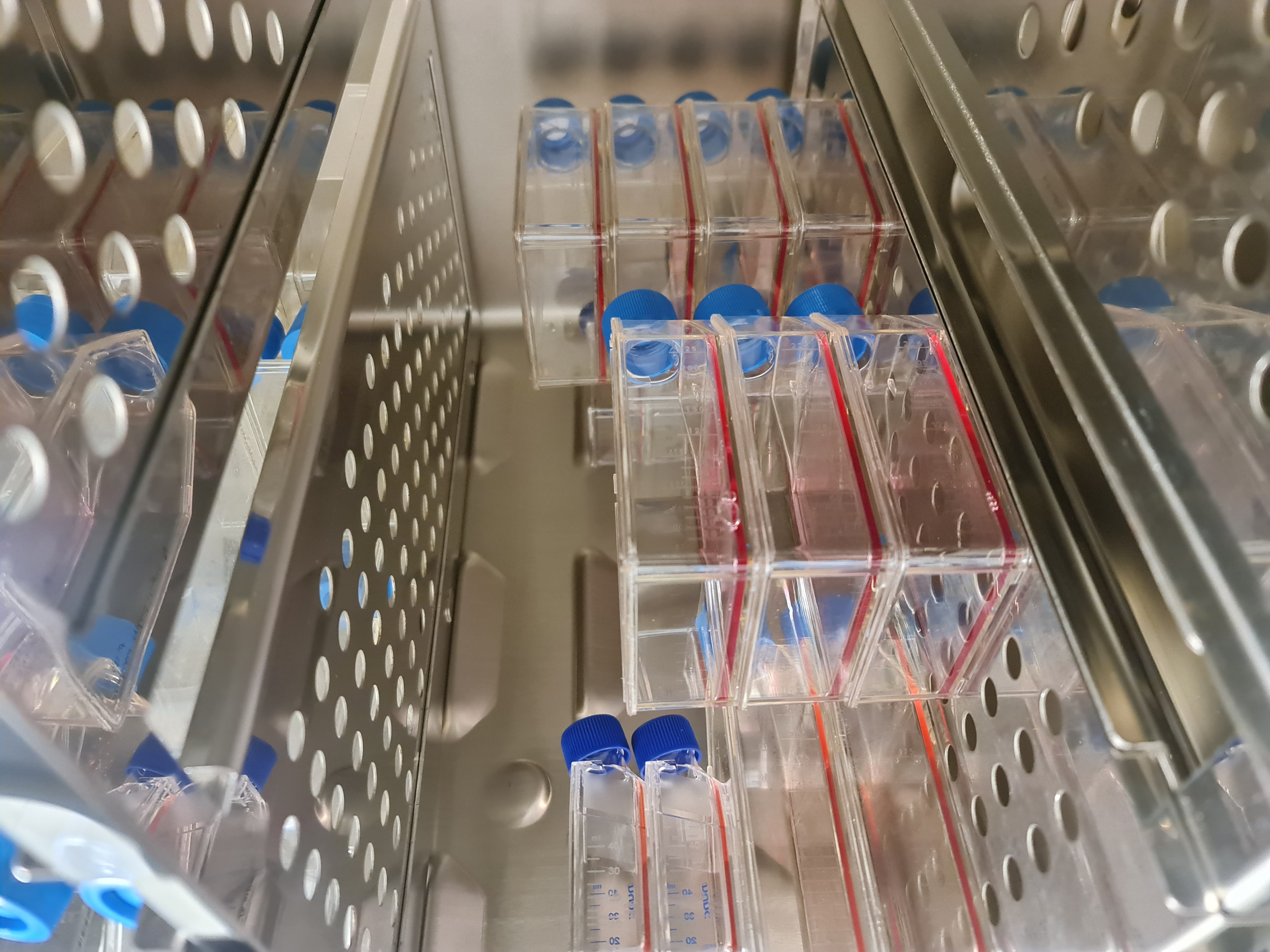
Cultivated cell cultures. Photo credit: personal archives
Correct me if I’m wrong, but there seemed to be a lot of focus on stem cells a dozen years ago. And now it seems that everything has calmed down. Is it true?
Scientific progress is occurring very fast, technologies are being developed very quickly, so there is always interest in a new direction. There was a time when there was a lot of interest in stem cells. I cannot answer whether there are now fewer groups of researchers who work with these cells. I don’t think so. In January, I’m just going to a conference in the USA to present stem cells as an advanced therapy option. The USA probably has the largest number of research groups and companies studying and evaluating the potential of stem cell therapy.
Of course, the regulatory issues of working with stem cells are problematic. I belong to the International Network of Translating Research on Perinatal Derivatives into Therapeutic Approaches (SPRINT). As far as I know, the possibilities of using stem cells are highly dependent on national regulatory rules, bioethical approvals for clinical trials, etc.
To answer your question, I think that the focus on stem cell research and therapeutic use has not disappeared, but only because of the progress in science, a new research object is discovered that was not known and studied until now, and then many people give themselves to the analysis of new research objects, they are given more financing.
What breakthrough in cancer treatment or understanding of cancer would be needed now to fundamentally change the way we understand and treat cancer?
As I’ve mentioned, many cancers are curable with existing protocol treatments, but not all cancers respond to them. Based on my research findings, I believe that both treatment and diagnostics will become increasingly individualised. That is, by evaluating the patient’s tumour tissue and molecular, epigenetic, etc., changes in it. And according to individually identified molecular changes, combination therapy will be applied. Of course, the financial issue will also be relevant here.
By the way, we carried out a project in which we investigated the expression of which genes could determine whether leukaemia might relapse. After thoroughly investigating this and identifying several related genes, we have submitted recommendations to the Ministry of Health of the Republic of Lithuania. I would say that it is my contribution to medicine as a researcher.
In October, you were nominated for the Lithuanian Science Prize for your cycle of research works. Can you tell us more about it?
Yes, we are nominated and participate in the competition for the award for the cycle of works in 2008–2022. The cycle is called “Investigation of the role of cancer and stem cells in the pathogenesis of diseases and their application for therapy - synergy of experimental biology and computer informatics”.
We synergise research in experimental biology with computational informatics. I have already told you about molecular research on cancer and stem cells, and we used computer informatics to process the results. Changes in human cancer and stem cell biomarkers and their levels are determined using numerical intelligence methods, machine learning and the development of new mathematical algorithms. Thus, numerical intelligence and mathematical modeling are applied to advance imaging and interpretation of molecular targets in cancer and stem cells.
Our work is submitted for the competition by Vilnius University together with Vilnius Gediminas Technical University, as we are co-authors of a cycle of four research works representing both universities.
Are you happy with this nomination? After all, it is a very high rating for a researcher.
Yes, of course, the mere nomination that we are evaluated and selected for this competition is very important. We really appreciate it and are glad to be noticed.
Interview by Goda Raibytė-Aleksa