Tissue Engineering: From Adam and Eve to the Artificial Heart
 By sharing knowledge and combining several fields of science, tissue engineering researchers will develop methods and products that will help treat pathologies or become an engine for further research, says Dr. Daiva Baltriukienė, Researcher at the Department of Biological Models, Institute of Biochemistry, Vilnius University (VU).
By sharing knowledge and combining several fields of science, tissue engineering researchers will develop methods and products that will help treat pathologies or become an engine for further research, says Dr. Daiva Baltriukienė, Researcher at the Department of Biological Models, Institute of Biochemistry, Vilnius University (VU).
Today, tissue engineering allows us to enjoy the first personalized medical products, transplant skin, or even engineer artificial organs. “Over the past 30 years, there has been a huge breakthrough in tissue engineering,” said Dr. D. Baltriukienė.
History of Tissue Engineering: Cells Crossing the ‘Iron Curtain’
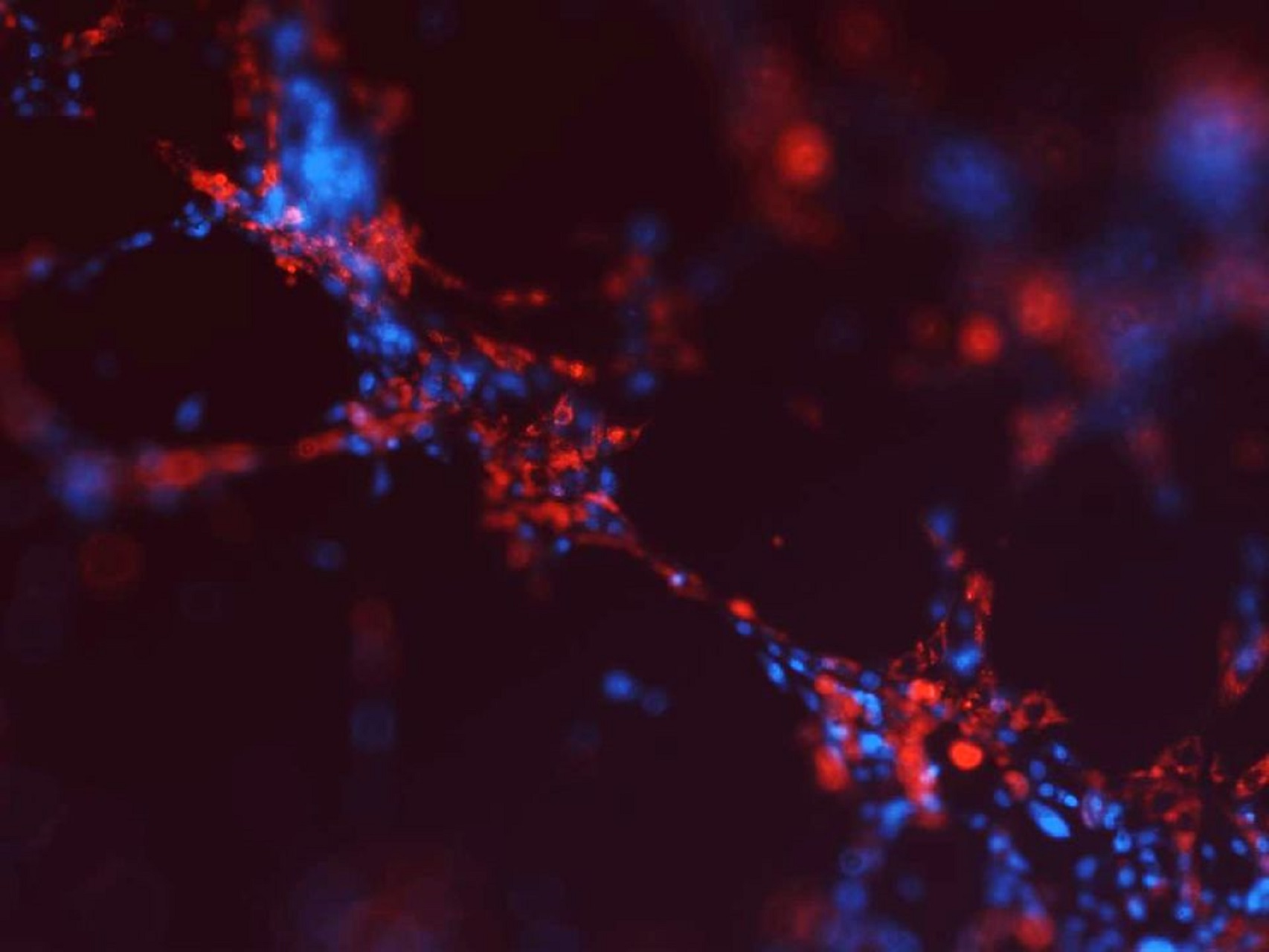
Dr. D. Baltriukienė jokes that tissue engineering can be traced back to Biblical times when Eve was created from Adam’s rib. However, real cell research began in the United States in 1907, when Ross Granville Harrison isolated fragments of neural tissue from a frog’s neural tube, inserted them into a hanging drop of lymph, and noticed that the cells were multiplying.
Despite this major breakthrough, more extensive research on cells could not be initiated at that time because a suitable artificial medium for their growth had not yet been developed. Intensive research to create a suitable medium for in vitro cell culture began in 1946. In 1955, Harry Eagle created a medium that is still in use today.
“In 1951, the first human cell line was isolated. The cells were obtained from the tumor tissue of a woman with cervical cancer and named HeLa after the first syllables of the patient’s name. George Otto Gey, a US scientist who isolated the cells, shared his discovery with scientists around the world: in around 1960, the cell line was sent to space by the first USSR satellites to prove that the cells proliferate better in zero gravity than in the state of gravity. So these cells even crossed the “iron curtain,” the scientist said. Interestingly, the cells are still being researched in many laboratories around the world.
In around 1960, hematopoietic (blood-derived) cells were obtained, the isolation of which led to a breakthrough in the stem cell area. Skeletal muscle cells were also isolated at the same time. US scientist Alexander Mauro proved that there is a population of cells in the skeletal muscle that, for example, migrate to the lesion area when cut and thus begin the healing process.
The VU researcher says that in an article published in the journal Science in 1993, US researchers Robert Langer and Joseph Vacanti presented three components needed to create artificial tissues: suitable cells that could form tissue; extracellular matrix that can be both natural and artificial; bioactive molecules that control the fate of cells, i.e., promote their proliferation, integration and differentiation in the desired direction.
“So we could say that the field of tissue engineering is relatively new, it’s only turning 30,” the scientist said.
Tissue Engineering at VU: Hopes for Treating Heart Diseases
Tissue engineering research at VU began with skeletal muscle stem cell research in 1998. 15 years ago, high hopes were placed on these cells to help develop new strategies for treating heart disease, as both heart and skeletal muscle are made up of muscle cells. The researchers hypothesized that skeletal muscle cells could become myocardial cells and restore damaged heart muscle after myocardial infarction when a large proportion of the cells die. At the time, the researcher and her colleagues were also conducting research into this type of cell to apply them in therapy.
“We started working with skeletal muscle stem cells, tried to implant them in an artificially engineered infarction area in the heart of a rabbit, and monitored whether the areas of damage would recover. Attempts were later made to form a cell sheet for transplantation by covering the area of necrosis in the heart. However, due to the chosen model, the research at that time was not very successful, and later other groups of scientists from around the world found that the therapy of these cells is not suitable for treating heart disease because it causes arrhythmias,” the scientist said.
In stem cell research, the concept of cell differentiation is often used to describe the type of cells - nerve, muscle, or bone - that will be grown from the stem cells in question. Dr. D. Baltriukienė and her colleagues carry out research, where they change the hardness and softness of the extracellular matrix in stem cells, which allows for regulating the further development of cells.
“If cells are grown on a very soft surface, they tend to differentiate into cells characteristic of nerve tissue. When they grow on a medium-hard surface, they differentiate into muscle or cartilage cells, and when on a very hard surface, into bone cells. Another property is the hardness of the tissue or organ, which depends on the ratio of proteins in the extracellular matrix. One of the most important proteins is collagen because when the ratio changes, the hardness of the tissue changes and it can no longer perform its function, which leads to diseases,” the scientist said.
Interdisciplinary Cooperation Opens Up New Possibilities
Dr. D. Baltriukienė admits that while the research of their group started with soft tissues, today, more work has been done to create hard tissue. In tissue engineering terminology, hard tissue refers to artificial bone tissue. In 2009, VU tissue engineers started cooperating with researchers at the VU Laser Research Center.
“Laser scientists had several materials that were promising in creating artificial tissues. We first evaluated whether their proposed solids are suitable for cell growth and how the cell behaves on artificial organic-inorganic polymers, how it grows in those polymers,” the scientist said.
Later started collaborations with dentists to create artificial bone, and VU tissue engineering researchers, in collaboration with researchers at the Faculty of Chemistry and Geosciences, sought to develop a polymeric material that could be used as a framework to create softer tissues than bone: cartilage, muscle, blood vessel.
“The idea came about while working with researchers at the Laser Research Center, when we encountered a rather sensitive methodological problem: laser technology is expensive and time consuming, and our studies required a number of uniform samples to obtain reproducible results. Thus, we used polydimethylsiloxane (PDMS) soft lithography. We attempted to evaluate whether PDMS could be used as a polymer for tissue engineering purposes. We were very surprised to learn that this polymer did not cause any inflammatory reaction when implanted in animals. The body responded better to it than to the surgical suture,” said Dr. D. Baltriukienė.
Despite its properties suitable for implantation, this polymer also had several drawbacks: cells clung to it but the interaction was short-lived, and the formation of a thicker derivative reduced its elasticity and it began to break: “In the project of the Research Council of Lithuania, we cooperated with the researchers of the Faculty of Chemistry and Geosciences, who tried to develop new polymers based on siloxane material. These new polymers were supposed to be suitable for constructing a tissue softer than bone. Several promising polymers have been synthesized.”
(Un)success of Stem Cells in the Beauty Industry
In terms of the practical application of tissue engineering, the greatest progress has been made in relatively simple tissues such as skin. In the case of a full layer of skin damage - from 1 to 4 cm, it does not heal on its own, so it calls for outside intervention.
“The first products registered for treatment were artificial skin constructs. The simplest method is to apply a sheet of artificial cells formed from keratinocytes to the damaged skin to promote skin recovery. Although the skin is a relatively simple organ, it still poses challenges: how to properly insert hair follicles and sweat glands, no less important are proper skin pigmentation and protection against ultraviolet rays. These issues are still being addressed,” she said.
Stem cells are also used in cosmetology to regrow hair or rejuvenate the skin.
“There has been a great deal of research around the world in recent years. Some recent research suggests that hair growth is better promoted by cell extracts rather than full stem cells, namely the liquid part of the cells remaining after the separation of their membranes. There is also a lot of work being done to try to use stem cells for hair replacement in the case of baldness, but so far we have little research results in this area,” Dr. D. Baltriukienė said.
Stem cells and their products are also used to rejuvenate the skin and reduce wrinkles. Unexpected and painful consequences can sometimes occur during these procedures.
“I have read about an incident where a patient was injected with mesenchymal stem cells to reduce wrinkles, but the cells differentiated into bone tissue cells and bone derivatives began to form in that area. This happened because the selected mesenchymal cells were in a very early differentiation stage and received signals to differentiate into bone tissue cells when injected,” the scientist said.
Tissue Engineering is the Key to Personalized Medicine
Although a great deal of research is being done in the field of tissue engineering, its results are so far applied to individual rather than routine treatments. The main organs and tissues that have already been engineered and implanted are skin, bladder, uterus, and bone tissue.
Significant work has been done to engineer an artificial heart, but the scientist notes that a completely artificial heart has not yet been engineered. “Scientists have already applied S. Yamanaka’s discovery to make skin cells capable of differentiating into any cell in the body. Using them, scientists have shown that it is possible to restore a damaged heart to make it functional, but so far, it is only a lab experiment,” Dr. D. Baltriukienė said.When it comes to organ implantation, one of the few areas where this process is routinely performed is the transplantation of large blood vessels.
“Large blood vessels are a bit simpler because their replacements are done routinely and do not require tissue engineering. Decellularized blood vessels can also be used for this purpose without creating immune reactions. The problem arises when we talk about the formation of smaller blood vessels (less than 6 mm in diameter). It is very difficult to create such small-diameter blood vessels and form and properly position the networks of venules and arterioles. If we want
to create bigger tissue, we have to ensure its functions, and innervation becomes the second big challenge,” the scientist shared her insights.
Tissue Engineering Research Responds to the Breakthrough in Biotechnology
Tissue engineering is a very promising field. We already have the first lab-engineered tissues and even organs, and there will be many more in the future. Dr. D. Baltriukienė recalls the tissue engineering development planned back in 2007 that pointed out that in 2019–2020, there will already be a fully operational tissue construct that can be implanted in the body. However, we do not yet have such a construct due to the lack of long-term data on how cells behave when implanted in the body; therefore, the biggest breakthrough is expected in the application of tissue engineering in personalized medicine.
“No less promising area is the development of models for medicine selection. Not only the principles of tissue engineering but also microfluidic technology would be used for that. This would allow for the development of very small tissue or even whole body models to ensure the efficient selection of bioactive compounds with therapeutic effects. The pharmaceutical industry is costly as there are very many stages to go through before the medicine reaches the consumer. Combining nanotechnologies, microfluidics, stem cell technologies, and tissue engineering principles can create new efficient ways to select medicine,” the scientist said.
From a modern perspective, the breakthrough in biotechnology also contributes significantly to the applicability and development of tissue engineering science.
“Over the past 30 years, there has been a huge breakthrough in tissue engineering. Following unsuccessful experiments, the scientists return to labs to create even more complete products and bring them closer to routine treatment. By sharing knowledge and combining several disciplines, tissue engineering researchers will develop methods and products that will help treat pathologies or become an engine for further research. But it takes time,” Dr. D. Baltriukienė said.